Phalloplasty Transgender Surgery
(FTM Bottom Surgery) in Palos Verdes
Everyone deserves to feel comfortable in their body and have their outward appearance reflect who they are inside. Transgender surgery encompasses a multitude of procedures that allow transgender patients to have physical characteristics and features that more closely match their gender identity. These procedures are also known as gender reassignment surgery, sex reassignment surgery, gender confirmation surgery, and gender-affirming surgery.
For female to male (FTM) transgender patients (transgender men) and non-binary patients, Dr. Boyd offers the FTM bottom surgery known as phalloplasty.
What Is Phalloplasty?
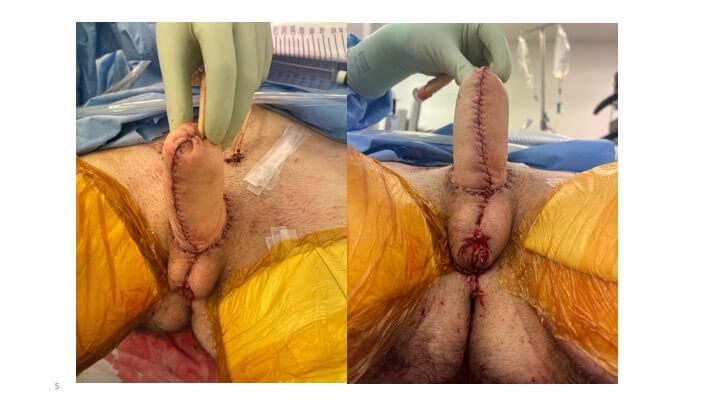
Phalloplasty is a procedure that creates a penis and lengthens the urethra. Dr. Boyd most commonly performs this genitourinary reconstruction surgery using a tissue flap from the patient's forearm.
For trans men, phalloplasty constructs a realistic penis that helps them realize their gender expression and transition socially. Cisgender males who have experienced physical trauma or medical issues that have affected their penis can also benefit from phalloplasty to restore the form and function of their penis.
What Can Phalloplasty Achieve?
A Natural-Looking Penis
Many patients wonder whether phalloplasty looks real. The goal of this procedure is to create a penis that appears physically realistic and natural.
Patients can rest assured that they will have a penis that looks natural, and no one needs to know they underwent phalloplasty unless they decide to tell them.
Standing Urination
Many trans patients are concerned about urinating through their phallus after FTM bottom surgery. During this procedure, the urethra is lengthened to the tip of the reconstructed penis.
This allows patients to urinate standing up once they have healed from surgery. In fact, the first goal of phalloplasty is to enable the patient to urinate standing without leaks.
Erogenous Sensation
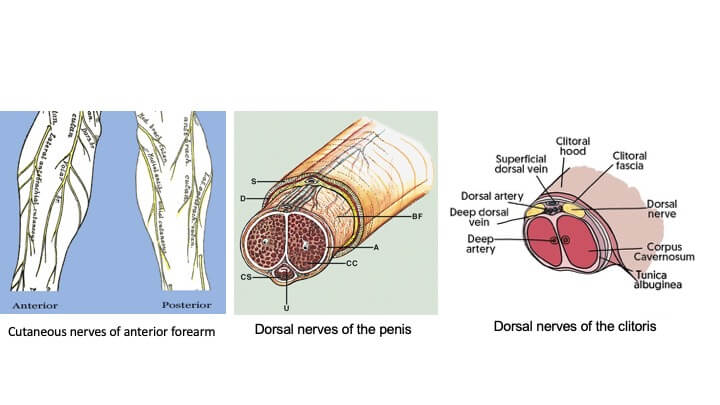
Patients may be curious about what they will experience in terms of sensation with their reconstructed phallus. Because the sensitive nerves from the forearm are joined to the nerves of the clitoris, patients experience erogenous sensory recovery.
This provides phalloplasty patients with the ability to feel sexual stimulation.
Penetrative Sex
Sex is a major part of most people’s lives and relationships, and patients often wonder if they will be able to have penetrative intercourse after transgender bottom surgery.
For patients who want the ability to have penetrative sex, a penile implant can be placed approximately one year after phalloplasty.
What Is Involved in Phalloplasty FTM Bottom Surgery?
What Is a Phalloplasty Consultation Like?
A consultation with Dr. Boyd and Dr. Gladys Ng is necessary before undergoing phalloplasty. Dr. Ng is a UCLA urologist specializing in transgender surgery. Phalloplasty, together with vaginectomy, scrotoplasty, and urethral construction, is a complex surgery requiring the expertise of different dedicated specialties.
During your consultation, Dr. Boyd and Dr. Ng will perform a physical evaluation and discuss your goals for the procedure to determine if you are a candidate.
TPatients undergoing transgender surgery must have been evaluated by specialists in gender health and have two letters of recommendation. They must also have lived as their gender identity for at least a year before undergoing gender reassignment surgery.
Once confirmed as a candidate, Dr. Boyd and Dr. Ng will create a personalized surgical plan based on your needs. At this time, you can ask any questions you have. You will also receive detailed pre-operative instructions to follow.
What Procedures Are Done Before Phalloplasty?
The transgender male will generally undergo hysterectomy (removal of the uterus) and salpingo-oophorectomy (removal of the ovaries and fallopian tubes) prior to phalloplasty.
The vagina remains in place because some of it will be needed in the urethral lengthening.
What Kind of Anesthesia Is Used During Phalloplasty?
To keep you comfortable throughout the procedure, phalloplasty is performed under general anesthesia. You will be asleep the entire time to ensure you do not feel any pain.
Phalloplasty Procedure
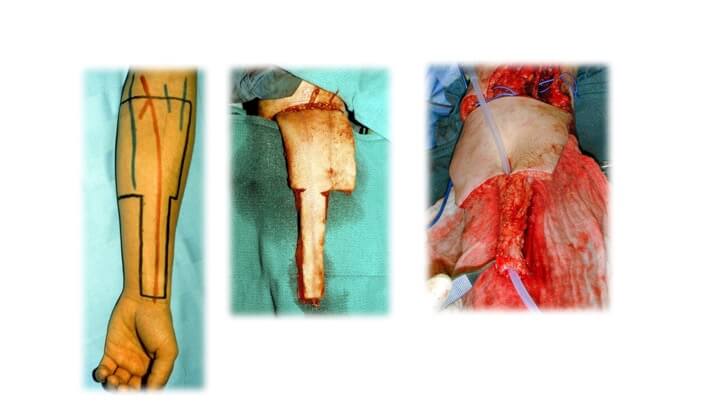
Older phalloplasty techniques using forearm skin require side-by-side flaps, one for the urethra and one for the skin cover. They are wrapped around each other like a jam roll to produce a tube within a tube. The arm defect thus becomes so wide that the donor tissue taken extends around the forearm and produces a severe, almost circumferential, deformity.
Dr. Boyd's "Cricket Bat" Flap Phalloplasty Technique
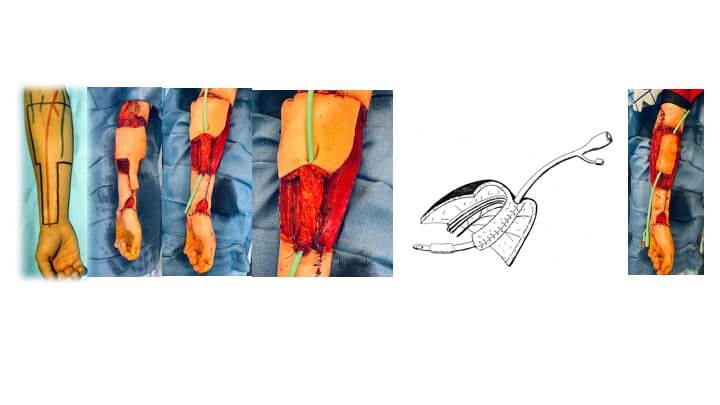
To avoid this, Dr. Boyd developed the “cricket bat" flap technique, with the donor tissue extending from the wrist crease to the elbow crease. The principle here is that the urethral portion is a narrow longitudinal extension (handle) of the skin portion (blade) and folds at the junction between the two. The scarring is thus confined to the front of the forearm, occasionally permitting the urethral defect to be closed directly without a skin graft.
The technique utilizes the least hairy portion of forearm skin, as the urethra and entire unit have a direct sensory supply by the anterior forearm nerves. The side-by-side technique, on the other hand, extends beyond the territories of these nerves, limiting the potential for sensory return.
The nerves of the forearm are attached to the clitoral nerves to create erogenous and tactile sensation, while the blood vessels are joined to recipient vessels in the groin to restore circulation.
Phalloplasty surgery takes approximately eight to 10 hours to complete.
How Is the Scrotum Created?
The scrotum is constructed from the labia majora, and the urethra is extended to the base of the phallus using local flaps from the labia minora and vagina. The vagina is otherwise removed.
What Can I Expect After Phalloplasty?
How Long Does It Take to Recover From a Phalloplasty Procedure?
After FTM bottom surgery, patients will need to remain in bed for about five days. This is to monitor the blood supply and ensure the reconstructed penis does not hang down and put the vessels on undue stretch. A sling must be worn to support the phallus until it is fully healed.
Two catheters will be in place, one emerging from the new urethra and another from just above the pubic bone. These will be used for six weeks after surgery to drain your bladder. Patients must take extra care not to pull on these catheters.
Is Recovery From Phalloplasty Painful?
Phalloplasty involves fairly extensive surgery, and most patients experience some level of pain and discomfort while healing. Dr. Boyd will prescribe medication to help manage the pain during your recovery.
Is Genitourinary Reconstruction Permanent?
Yes, your phalloplasty results should be permanent and last your entire lifetime. If you have any concerns about the procedure’s results, you can discuss these details with Dr. Boyd.
Will My Penis Function After Surgery?
Yes, your reconstructed penis is designed to be functional after your procedure for both urinary and sexual activities.
Can I Have Penetrative Intercourse After Phalloplasty?
Most patients need a penile implant to allow the penis to become erect enough for penetrative intercourse. The procedure to insert the implant is done approximately one year after phalloplasty.
Patients will need to wait a few weeks after receiving the penile implant to engage in penetrative sex.
Frequently Asked Questions About Phalloplasty
Some of the common traits of an ideal phalloplasty candidate include being:
In overall good health
A non-smoker or willing to stop smoking before and after the procedure
Realistic in his expectations for the surgery
Trans patients will need letters of recommendation from specialists in gender health.
Patients interested in penis reconstruction can consult with Dr. Boyd to determine whether they are a viable candidate for the procedure.
While the majority of patients who undergo phalloplasty are transgender or non-binary, cisgender men may need genitourinary reconstruction to correct post-traumatic penile defects or penis amputations. The forearm tissue flap can also be modified to deal with partial defects of the penis and penile urethra.
Cisgender males may undergo phalloplasty after:
An accident or injury affected their penis/genitals
Cancer of the penis that required amputation or partial amputation
Diseases or infections such as synergistic gangrene (Fournier’s gangrene)
Other conditions that impacted the male genitals
The cost of phalloplasty depends on the surgical techniques used and the extent of reconstruction needed. Patients undergo phalloplasty for various reasons and have individual needs that may affect the cost of their penis reconstruction. To find out your specific phalloplasty cost, please schedule a consultation with Dr. Boyd.
The majority of insurance companies cover the cost of phalloplasty. It is illegal for private insurance providers to deny coverage for medically necessary transgender surgeries, and reconstructive procedures are generally covered by insurance.
Dr. Boyd can negotiate with your insurance company to help get you coverage, if needed.
Dr. Boyd will determine which parts of your surgery should be performed on an outpatient or inpatient basis based on your unique circumstances. However, the majority of patients get their initial phalloplasty on an inpatient basis.
When you are released to go home, it can be very helpful to have someone to help you with basic chores and tasks around the house.
For most of Dr. Boyd’s 30 years in practice, he has been interested in genitourinary reconstruction (phalloplasty). Dr. Boyd is a phalloplasty surgeon and microsurgeon who understands the needs of transgender patients. He is part of UCLA's Gender Health Program and works with Dr. Ng and a team of other LGBTQ Champion physicians.
Dr. Boyd was faced with a problem early in his career: a young married man lost his penis to flesh-eating bacteria after a circumcision. As a microsurgeon, Dr. Boyd was asked to develop a one-stage reconstruction of the penis and urethra.
He designed a flap based on the forearm that folded on itself and called it the "cricket bat" flap. The handle portion folded in and was tubed to form the urethra, while the wider ‘blade’ portion wrapped around the urethra to form the skin on the outside of the new penis. Blood vessels were reconnected to restore circulation, and nerves were reattached to provide sensory recovery. The use of this construct with penile implants enabled the individual to subsequently father a child.
Since then, Dr. Boyd has successfully used this technique for numerous female to male (FTM) transgender patients and taught other surgeons how to perform it.
Dr. Boyd specializes in phalloplasty, but he also offers removal of the breasts (FTM top surgery), which is performed similarly to breast reduction surgery.
Dr. Boyd works closely with Dr. Gladys NG at UCLA Medical Center, who performs various vital associated procedures such as vaginectomy (removal of the vagina), scrotoplasty (scrotum construction), and insertion of testicular implants. She also handles catheter management and deals with leaks should they arise. This is in addition to an extensive practice with vaginoplasties (creation of a vagina) in trans females.
Hysterectomies (the removal of the uterus) and salpingo-oophorectomies (the removal of the ovaries and fallopian tubes) may be performed before a patient’s phalloplasty by the gynecologists on the team.
Non-binary patients may wish to retain their female reproductive parts. In that case, penis reconstruction can be performed by itself, usually without a urethra.